We benefit from learning more about the wonders of the human body. Wellness always begins with our lifestyles: what we eat, how we move, and how we navigate the complexities of modern living. Aging is part of our lifespan - there is only one escape! I became curious about what happens to our bodies as we age and what strategies we can employ, given our access to wisdom, common sense, technology, and scientific information. Each month, I will feature an article on the aging human body. I am not a medical professional, and that’s a good thing because I write so my readers can easily understand.
What our bones do for us:
Provide a rigid framework for the rest of our body parts
Contribute to our ability to move
Protect some of our internal organs: skull/brain, ribs/heart, lungs)
Stores and regulates minerals that can be released as needed
Blood cells are formed in our bones
Five Facts about Our Bones:
We are born with 300 bones but end up with about 206.
Our hands, wrists, and fingers have 54 bones.
The longest bone is our femur (thigh bone).
The shortest bone is our stirrup-shaped stapes in our middle ear.
The funny bone (nothing funny about the pain) is not a bone but the ulnar nerve that begins at the elbow.
Osteopenia & Osteoporosis
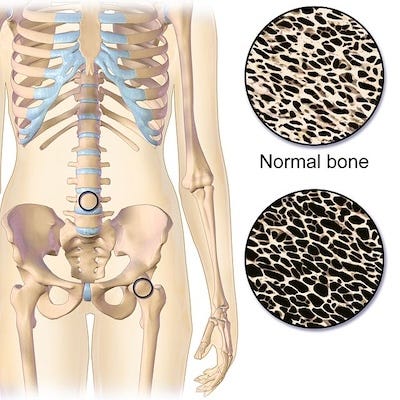
As we age, our bones become weaker, losing minerals like calcium that make up our bones. Bones are dynamic tissue that continually replenish lost bone cells. Bone loss occurs when the body eliminates more cells than it is creating. Osteopenia (osteo = bone; penia = deficiency) can be considered the first stage of osteoporosis (porosis = cavity formation, porous). Half of Americans over 50 have some degree of osteopenia. About 20% of American women have osteoporosis.
The risks for osteopenia, osteoporosis, and bone fractures increase significantly for people over age 50, especially for post-menopausal women. Estrogen is essential for bone health, ensuring calcium absorption into the bones. Estrogen declines after menopause, and bones can quickly become porous, putting older women at a higher risk for bone breaks. The most common bone fractures are wrists, hips, and vertebra. Osteoporosis is a major factor in the disability of elderly women. Hip fractures can be life-changing because many older people can no longer live on their own even after recovering from one.
It’s called a silent disease because it’s gradual and painless, with no symptoms to diagnose. Risk factors include aging, having a family history of diagnosed osteoporosis, ethnicity, and rheumatoid arthritis. Lifestyle factors like smoking, alcohol, insufficient exercise, poor nutrition, and low dietary intake of calcium can significantly increase the risks of decreased bone density.
Bone Density Tests
There is a lack of consensus on the regular use of a bone density test, a low-level X-ray that measures the gram levels of bone minerals. Some physicians automatically recommend a bone density test for all post-menopausal women; others wait until women are in their 70s and/or have experienced a fracture. If there is evidence of minimal bone loss (called osteopenia), they might prescribe an expensive drug that can include unpleasant side effects and/or recommend lifestyle modifications to reduce bone loss by increasing cell production.
What is a bone density test and score?
Prevention remains the best strategy for reducing osteoporosis. The first steps to building and maintaining bone density are incorporating healthy and nutritious foods and daily exercise.
Caution: If you have been diagnosed with osteoporosis, check with your healthcare provider about the types of movement you should avoid. The Mayo Clinic offers some tips.
Lifestyle Modifications
Don’t wait to nourish your bones: the younger you start, the better.
Daily weight-bearing exercise sessions like walking, running, hiking, stair-stepping, tennis, and dancing are essential to building and maintaining strong bones. Regular exercise helps to produce stronger bones. (See my caution above.)
Yoga and certain martial arts utilize your weight for strength-building in specific areas of the body.
Recommended daily amounts of 1200 mg of calcium and 320 mg of magnesium for women over 50, consumed preferably through diet.
Daily sunlight exposure for vitamin D (Bare arms and upper torso, but that’s not reasonable in winter…is it?)
Smoking, alcohol, soda pop, excessive salt and sugar, excessive caffeine, and certain medications can contribute to bone density loss.
Eat more brassicas, leafy greens, nuts, seeds, whole grains, and beans. Dairy products are rich in calcium but not easily absorbed, so don’t rely on dairy as your sole source of calcium.
Increase the daily amount of healthy protein through legumes, nuts, seeds, fish, and lean meats.
Increased phytoestrogen intake may help reduce bone loss and build new bone.
Nutritive Herbs
Some studies suggest that phytoestrogens help bone loss in aging women. Weekly nourishing herbal infusions are one easy way to incorporate bone-building minerals and phytoestrogens.
What’s a nourishing herbal infusion?
A nourishing herbal infusion is a tea made with nutrient-dense herbs. Infusions are steeped in just boiled water for 4-24 hours to extract minerals and vitamins from the herbs. Infusions are typically made with one ounce of herbs in a quart jar or French press, covered with hot water, and steeped for at least four hours. The herbs below are ideal for nourishing infusions. I drink a combination of these plants somewhat irregularly because they are not the tastiest drinks around.
Always check with your pharmacist or healthcare provider for possible drug-herb interactions before using herbs medicinally or nutritionally.
Alfalfa: Contains both minerals and phytoestrogens (research for side effects and drug interactions before use)
Horsetail: All about the silica
Nettle: calcium-dense with magnesium, potassium, and iron
Oatstraw: High levels of calcium, magnesium, and silica
Red Clover: Lower levels of minerals but contains phytoestrogens

Osteoarthritis
I am among the 33% of Americans over the age of 65 who are afflicted with osteoarthritis. In the last few years, I noticed that the knuckle on my right forefinger has morphed into a bony knob, and the joint at my wrist and thumb is enlarging and aches after a few hours of repetitive use, like pruning in my garden. Last year, x-rays revealed minor arthritis in my lower spine and hip joints.
Osteoarthritis (also known as degenerative joint disease) is the most common type of the 100 types of joint inflammation. The effects of arthritis vary widely from occasional flare-ups to debilitating chronic pain. It’s considered the number one disability in the United States, and it contributes to additional health problems because pain reduces physical activity. Diagnosing the type of arthritis is an important first step; the symptoms can be similar for various joint inflammation diseases, but the causes and treatment can differ. For example, osteoarthritis is not the same as rheumatoid arthritis, a disease caused by the immune system mistakenly attacks healthy cells.
Osteoarthritis is typically associated with the aging process, the wear and tear on our bodies, and, for some, old athletic injuries or physical trauma. It is also influenced by sex, genetics, ethnicity, and lifestyle. Recently, a new study found that low-grade inflammation may cause or increase its progress. Osteoarthritis affects the cartilage, the tissue that acts as a padding between the bones in our joints. It slowly disappears, resulting in what is commonly called “bone on bone.” Swelling and joint pain are the early indicators of osteoarthritis, and an x-ray is used to confirm. Unfortunately, considerable damage has been done by the time an x-ray is done.
Symptoms of osteoarthritis include:
Soreness and tenderness
Stiffness, especially after sitting or sleeping
Redness and warmth
Swelling caused by inflamed tissues
Bony proliferation on knuckles, causing them to look knobby
Lost range of motion
Poor sleep due to pain
Modern medicine usually recommends the standard pharmaceutical treatment: acetaminophen for pain and aspirin, ibuprofen, and naproxen for pain and inflammation. This protocol can help with the occasional flare-up, but osteoarthritis tends to worsen with age, especially if lifestyle factors are not modified.
In addition, there are side effects with over-the-counter (OTC) drugs, especially if taken daily: acetaminophen can cause problems with the liver, and nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen can create chronic digestive problems.
To succeed in life you need three things: a wishbone, a backbone, and a funny bone.
Reba McEntire
Lifestyle Modifications
As common as osteoarthritis is, the medical community does not fully understand how to prevent or cure it. Still, it has identified specific lifestyle behaviors to help delay and reduce its painful effects:
A healthy diet
Extra Virgin Olive oil: Human, animal, and lab experiments have shown that the polyphenols in EVOO effectively combat inflammation and improve arthritis symptoms in joints and throughout the body. The Arthritis Organization offers free articles and e-books on the benefits of a healthy diet and olive oil.
Daily weight-bearing exercise & stretching
Maintain a healthy weight (extra weight increases stress on knees and hips)
Ensure adequate sleep and rest for the body to recover
Strengthen muscles around joints for added support (especially the core muscles)
Avoid excessive repetitive movements
Some natural remedies for arthritis include applying heat to stimulate circulation and using cold to reduce inflammation and numb pain. Physical therapy and heating pads can also help manage pain. (I keep a large heating pad on my living room chair, using it once or twice a day on my back.)
Medicinal Herbs
One of the benefits of herbal remedies is that they generally have no adverse side effects. Another benefit is that there are a variety of herbs and applications to consider. The external use of herbs for pain and inflammation is generally safe, but users should be watchful of any reactions and stop using them if they become present. Always do ample research and check with your healthcare practitioner before ingesting herbs for medicinal purposes. If using pharmaceutical drugs, check with your pharmacist or healthcare practitioner for possible herb-drug interactions.
Caution: The FDA does not regulate herbs and other supplements, and the quality of these supplements can vary. Increasingly, inexpensive herbs are adulterated with similar-looking substances. Look for organic and third-party certifications when shopping.
Herbs: Topical Applications
Arnica: Arnica is used for topical (only) pain relief and as an anti-inflammatory. It can be made or purchased as a topical cream or gel. Several studies have found it effective for pain in the hands and knees. Avoid using it on open wounds or cuts.
Cayenne: Capsaicin, a major constituent of cayenne peppers, blocks substance P, which sends the message of pain to the brain. Commercially made capsaicin topical creams are widely available, but cayenne salve is easy to make.
Stinging Nettle: I first learned about nettle’s historical use for arthritic pain relief when I presented a lecture years ago and discussed nettle’s nutritional and medicinal value. An older woman approached me during the break from a presentation I was offering on medicinal herbs. I immediately recognized her swollen and knobby hands as signs of arthritis. She had developed arthritis as a child, and her country doctor told her to head out to the nettle patch and rub her hands with the stinging leaves. She said her pain disappeared for days at a time. It's not the most pleasant way to alleviate arthritic pain but has a long history of use.
Willow Bark: Willow bark contains salicin and has been used for thousands of years for multiple purposes. As the precursor to manufactured aspirin, it can be used topically to relieve arthritic pain. Commercial willow liniments can be purchased, but they are easy to make.
Lavender and olive oil: Add 20-30 drops of lavender essential oil to 1 oz of olive oil and use for mild knee pain.
Herbs: Internal Uses
Ashwagandha: This amazing plant can offer multiple benefits to people with arthritis. Regular use can help calm the nervous system, support restful sleep, soothe pain, and reduce inflammation.
Stinging Nettle: Taken as an extract, nettle can reduce inflammation.
Turmeric: This current “super” herb has a long history of use for various conditions. Curcumin, a major turmeric constituent, decreases pain and inflammation and has been used for chronic joint problems.
Collagen Supplement: Research results are mixed on using collagen for osteoarthritis pain, but its use shows promise.
What are you doing to maintain bone health? What have you found most effective in managing the pain of osteoarthritis?
Thank you for being here. All of my posts are free, but if you’d like to support my work, you can do so by:
Liking and restacking this post so others are encouraged to read it.
Share this post via email or on social media.
Taking out a paid subscription to this Substack.
Comments are always welcome.





Sue, thanks for compiling and presenting all of this useful information! My latest bone scan says I have osteoarthritis, but I don't have pain or swelling, and I walk about six miles a day between my daily activities and my planned hikes on the trails here. I do yoga, work in the garden, fix stuff around the house, climb on the roof occasionally, throw my western saddle on a horse about once a week and take a half-day ride, and so on. So I have to wonder if the bone scan was wrong or if my skeleton is just that far off the charts (I have always been slender with very small bones). Regardless, I'm going to take your suggestions to heart and continue living healthfully for as long as I can. :)
Sue, thank you for much good information in this post. I do a few things to help my aging body. I live in a 2-story house and make the trip up and down the stairs many times a day, often carrying books or baskets of clothing or knitting, etc. I have also placed a few things that I use daily on upper shelfs that I have to stretch to reach. Things like my daily teas, and coffee mugs, bathroom towels and washcloths and the kitty food is in a cannister on a bottom shelf. This little bit of stretching daily is certainly worth the effort. I also mow a good-sized lawn and rake and haul the leaves in the fall. Like you I love to garden. Because getting up from the ground can be difficult, I keep a lightweight yard chair and/or a gardening fork nearby to lever myself up and down. And sometimes to perch on the chair while pruning bushes or tying plants to stakes, etc. Little things like this keep me out there!
I do benefit from an occasional cup of stinging nettle or ashwagandha tea. And I can recommend Topricin's Fibro Cream that includes arnica as a topical pain reliever. It is especially helpful to get a good night's sleep when pain flares up. As I avoid dairy, in addition to daily vitamins I make a special effort to add vegies like chard and kale to my diet for the calcium and other healthful benefits. Adding a small handful to soups or casseroles is easy to do and tastes good, too. And lastly, throughout the winter I make my own sprouts! Usually alfalfa sprouts, but sometimes mung or radish. These sprouts are good on salads and sandwiches and the mung sprouts are terrific for egg foo young!