We benefit from learning more about the wonders of the human body. Wellness always begins with our lifestyles: what we eat, how we move, and how we navigate the complexities of modern living. Aging is part of our lifespan - there is only one escape! I became curious about what happens to our bodies as we age and what strategies we can employ, given our access to wisdom, common sense, technology, and scientific information. Each month, I will feature an article on the aging human body. I am not a medical professional, and that’s a good thing because I write so my readers can easily understand.

Digestive Health
In a 2022 survey by the American Gastroenterological Association, 40% of adults reported digestive complaints that have affected their daily activities like exercising and socializing. The modern lifestyle of ultra-processed foods, fast food drive-through fare, eating on the run, and overeating as a result of stress or addiction to fat and sugar has developed a corresponding number of digestive complaints: bloating, heartburn, indigestion, gas, stomach cramps, and diarrhea. Stress and anxiety can amplify many of the symptoms. Without lifestyle changes, our digestive system can eventually become chronically irritated and inflamed, resulting in conditions like gastritis, leaky gut, ulcers, gastroesophageal reflux disease (GERD), and inflammatory bowel disorders. Some of these conditions can contribute to the malabsorption of food, creating nutrient deficiencies.
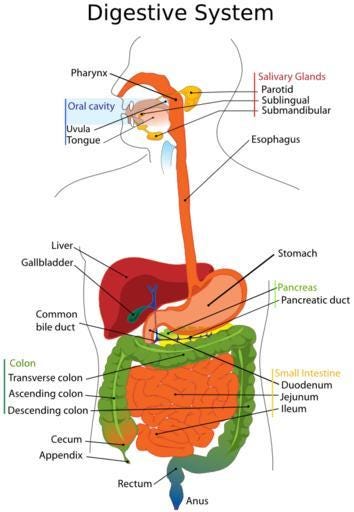
First, a quick review of our gastrointestinal tract’s highly efficient and remarkable anatomy and physiology.
From mouth to anus, our digestive system is 30 feet long! There are eight organs, each with specific functions:
Mouth - Saliva production (up to 1 liter per day) and food breakdown by chewing.
Esophagus - A muscular tube that moves food down our throat to our stomach using muscular contractions called peristalsis.
Stomach - A muscular organ that supports digestion with the aid of enzymes & acids.
Liver - Bile, a fluid that helps with digestion and carries waste, is created in the liver and stored in the gallbladder.
Gallbladder - Bile is released to digest fats and Vitamin K in the colon.
Biliary Tract - A series of vessels and ducts that move bile to the small intestine.
Small Intestine - The primary organ for the absorption of nutrients.
Large Intestine (the colon) - The primary organ for elimination.
Aging Digestion Facts
As we age, our digestive systems experience physical changes:
Digestive juices are reduced.
Saliva has fewer digestive enzymes.
The stomach produces less gastric juices, and its mucous lining degenerates.
Both the liver and pancreas reduce enzyme concentrations.
The muscles of the entire digestive system weaken, slowing movement in the digestive process.
The intestines lose elasticity, and their lining thins.
The intestines and colon become less efficient.
Many digestive complaints could be discussed here, but most are symptomatic of underlying causes associated with lifestyle choices and are not necessarily age-related. I selected the problems most often associated with an aging digestive system.
Constipation
Constipation is a symptom of an imbalance in the digestive system and can happen to anyone occasionally. Older people tend to experience constipation more frequently and even chronically. As noted earlier, the colon moves less efficiently, so feces may remain longer in the colon, allowing more water to be absorbed than usual, creating harder and drier feces. Other contributing factors for chronic constipation include:
A diet low in fiber and whole foods
Food sensitivity
Failure to hydrate regularly with water
Taking too many over-the-counter laxatives
Pharmaceutical medications, including opiates, antihypertensives, certain antidepressants
Over-the-counter products like antihistamines, antacids, and iron supplements
Lack of exercise and movement; prolonged bed rest
Resisting and delaying bowel movements
Certain medical conditions like stroke, diabetes
Possible blockage within the intestine
Monitoring your feces regularly can help indicate digestive health. The Bristol Stool Chart classifies stools by their appearance. Type 1 indicates severe constipation, while type 7 suggests severe diarrhea. Types 3 and 4 are typical, with 4 being the ideal “sausage” shape and smooth texture. Regularity of bowel movements, transit time from mouth to anus, and the color of feces are also used to identify potential issues.
Peptic Ulcers
Gastrointestinal ulcers are a fairly common condition in older people, and multiple factors contribute to their development, including a poor diet, high stress levels, continual use of anti-inflammatory drugs (NSAIDs), the stomach bacterium Helicobacter pylori, and digestive changes. Bleeding peptic ulcers require immediate medical attention as the mortality rate rises significantly with age.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) is often called acid reflux, while chronic, occasional gastroesophageal reflux is commonly known as heartburn. GERD is the most common digestive disorder seen in older people, and though they often have fewer symptoms, the disease presents more complications and severity of complaints. GERD occurs when stomach acid backs up into the esophagus, causing a burning sensation. This digestive disease can cause a loss of sleep and appetite, and if the stomach acid is inhaled into the lungs, it can create chronic respiratory problems. Risk factors include obesity, alcohol use, smoking, restrictive clothing, certain medications, and sleeping flatly.
Diverticular Disease
About half of people aged 60 and older have diverticulosis (i.e., little sacs on the intestine walls), which is associated with the aging of our colons. Diverticulitis occurs when small pouches in the colon's lining bulge along weak intestinal wall spots and become inflamed. Symptoms include gas, bloating, cramps, constipation, and abdominal pain.
Polyps
As we age, the risk increases for developing polyps, or small growths, in the colon. They can be predictors for cancer, so they are often removed during colonoscopies.
Gallbladder Disease
Inflammation of the gallbladder and gallstones are the two most common conditions associated with gallbladder disease. The risk for gallbladder disease increases significantly after age 40. Gallstones are hardened deposits of bile secreted from the liver and stored in the gallbladder. Some stones are called silent stones because they don’t show any noticeable symptoms; some stones can cause severe pain in the upper right abdomen and shoulder. Risk factors include age, ethnicity, family history, sex, obesity, and sedentary lifestyle.
Lifestyle
Diet is the most crucial factor in digestive health. High-fiber foods can help prevent constipation and ease symptoms of diverticulosis. Limit intake of bad fats, eat smaller portions and avoid processed and fast foods.
Nutrient-dense, antioxidant, and anti-inflammatory foods will support a healthy digestive system:
Leafy greens
Cruciferous vegetables
Alliums: garlic and onion
Whole grains
Omega-3 fatty acids: wild-caught salmon, trout, sardines, walnuts, flaxseeds, eggs
Colorful berries and other fruits
Culinary herbs and spices: turmeric and ginger are excellent
Enjoy eating in a relaxed setting, eating slowly and chewing thoroughly. If you eat fast, try setting the fork between each bite.
Exercise and movement at least five days a week supports overall health and specifically helps with elimination.
Maintaining a healthy weight can help prevent many age-related digestive problems.
Pharmaceutical and over-the-counter drugs can create problems within the digestive system. Avoiding health problems can reduce the number of medications you need to take, which means less opportunity for digestive side effects to develop.
Herbs
Medicinal herbs have a long history of successful use with digestive disorders. They can provide relief of discomfort, protect and soothe irritated tissues, stimulate digestive juices and bowel movements, ease muscle spasms, increase bile flow, and tone and strengthen the liver.
Chamomile (Matricaria recutita): Well known as an herb used to relax, chamomile is a powerful ally for common digestive complaints because of its healing effects on the gastrointestinal mucosa. It is helpful for indigestion, heartburn, flatulence, gastritis, spasms, and mouth ulcers.
Fennel (Foeniculum vulgare): As a carminative, fennel aids digestion and can ease cramping by relaxing the digestive muscles. In a 2006 study of nursing home patients who had chronic constipation, a commercial tea blend that included fennel, senna, coriander, and ginger proved effective among the patients.
Psyllium (Plantago ovata): Long used in commercial bulk laxatives, psyllium seed husks are an excellent source of soluble fiber. It can speed up food's travel time in a sluggish digestive system, can resolve diarrhea, and has proven helpful for irritable bowel diseases. Before using psyllium, there are some precautions to consider, so checking with a health practitioner is recommended.
Mallow (Althaea officinalis): A cooling and soothing demulcent herb (relieves irritation and inflammation), mallow has a long history of relief for problems with the digestive tract, including heartburn, constipation, and ulcers.
Herbal and Food Bitters: The taste of bitters is lost from some of our modern diets, but it serves an essential purpose in the overall health of our digestive systems. The bitter taste stimulates our digestive juices (saliva, enzymes, acids, bile, pancreatic hormones), which contribute to the breakdown of our food, ensuring the absorption of nutrients. The European tradition of eating bitter greens or drinking an aperitif before a meal is rooted in this understanding, and incorporating them into your diet is the ideal way to introduce bitters to your digestive system. Herbal bitters are liquid extracts of bitter herbs, and drinking a small amount before each meal can also increase digestive secretions. Bitters can be purchased online from herbal product suppliers, or you can make your own.
Note: The microbiome in our “gut” plays a critical role in both our digestive health and our overall wellness. I will dedicate a separate article to it.
Thank you for being here. All of my posts are free, but if you’d like to support my work, you can do so by:
Liking and restacking this post so others are encouraged to read it.
Share this post via email or on social media.
Taking out a paid subscription to this Substack.
Comments are always welcome.






Travel causes constipation for many of us. All the hydration, activity, and fiber in the world does not help me when I travel. On my next trip, I will be availing myself of Miralax at least every other day and would like to know what helps others in this situation.
It will sound strange, but a few years ago I had a rather sever case of the flu and in the long run it was the best thing that has happened to me in a long time. I couldn't hold down any food for a few days and only the smallest amount of things like applesauce or ginger ale for most of the following week. As I started to recover I felt weak, but I actually felt better. In part this was because I had just lost a good bit of weight and I had not started filling up on processed foods. It was a wake-up call. My appetite was still small and I chose a habit of small healthy meals. My motto was/is Fresh and Less. It took waking up to how much better I felt, to be able to stick to a healthy diet. Now I have no interest in overeating, no matter what the temptation might be. Less keeps me much happier. And Fresh is so much better for my brain, body and energy.